What is the Most Effective Treatment for Myasthenia Gravis?

Myasthenia gravis is a chronic autoimmune condition that affects the communication between nerves and muscles, often leading to weakness in the voluntary muscles of the body. For those diagnosed, the first question is often: what is the most effective treatment for myasthenia gravis?
While there’s currently no cure, a range of treatment options helps to reduce symptoms and improve quality of life. This article outlines the most commonly used myasthenia gravis treatments, how they work, and what to expect.
Understanding Myasthenia Gravis
Before looking at the available treatment for myasthenia gravis, it’s important to understand how the condition affects the body. In myasthenia gravis, the immune system mistakenly produces antibodies that block or destroy acetylcholine receptors at the neuromuscular junction. This disrupts the signals that trigger muscle contraction.
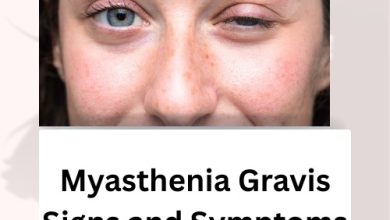
Symptoms can vary in intensity but typically include:
- Muscle weakness that worsens with activity
- Drooping eyelids (ptosis)
- Difficulty swallowing or speaking
- Shortness of breath
- Generalised fatigue
Since these symptoms can mimic other neurological conditions, accurate diagnosis is key before starting any treatment of myasthenia gravis.
Treatment Options for Myasthenia Gravis
Treatments for myasthenia gravis focus on improving communication between nerves and muscles, managing immune responses, and reducing antibody production. While conventional therapies are essential, some individuals also explore Natural Remedies for Myasthenia Gravis as complementary options. The right treatment approach often depends on symptom severity, age, overall health, and response to previous interventions.
Here’s a breakdown of the most widely used methods:
1. Acetylcholinesterase Inhibitors
First-line treatment for myasthenia gravis typically involves acetylcholinesterase inhibitors, most commonly pyridostigmine (Mestinon). These medicines work by preventing the breakdown of acetylcholine at the neuromuscular junction, enhancing the transmission of nerve signals.
Benefits:
- Quick symptom relief (within 30–60 minutes)
- Non-immunosuppressive
- Can be used long-term
Limitations:
- Effects are temporary and require multiple doses daily
- May cause side effects like stomach cramps, diarrhoea, or sweating
2. Immunosuppressive Therapy
For more severe or generalised cases, myasthenia gravis treatment often requires suppression of the immune system. Common options include:
- Corticosteroids (e.g., Prednisolone)
These reduce inflammation and antibody production. Patients typically start on a higher dose and taper down once symptoms improve.
- Steroid-sparing Agents
- Azathioprine
- Mycophenolate mofetil
- Methotrexate
These are used to reduce reliance on corticosteroids and help with long-term disease control.
Pros:
- Effective for moderate to severe cases
- Can maintain remission
Cons:
- Risk of infections
- Liver and bone marrow monitoring needed
- Takes weeks to months to reach full effect
3. Thymectomy (Surgical Removal of the Thymus)
The thymus gland plays a role in immune system regulation, and in many patients with gravis myasthenia, it’s abnormally large or has a tumour (thymoma). Thymectomy is often considered in patients under 60 or those with generalised symptoms and thymic abnormalities.
Benefits:
- Can lead to long-term symptom improvement
- May reduce or eliminate the need for medication
- Particularly effective for patients with early-onset disease
Risks:
- Surgical complications
- Hospital stay and recovery time
Thymectomy isn’t suitable for every patient but remains an important treatment of myasthenia gravis in selected cases.
4. Monoclonal Antibody Therapy
Recent advancements have brought targeted treatments into the mix. Monoclonal antibodies like eculizumab (Soliris) and ravulizumab (Ultomiris) block specific parts of the immune system responsible for the disease process.
These therapies are primarily used in refractory generalised myasthenia gravis – patients who don’t respond well to conventional treatment.
Advantages:
- Targeted and specific action
- Fewer side effects compared to broad immunosuppressants
- Improves muscle strength and reduces flare-ups
Disadvantages:
- High cost
- Requires intravenous infusion
- Long-term effects still being studied
5. Plasmapheresis and Intravenous Immunoglobulin (IVIG)
Used during myasthenic crises or to quickly improve symptoms, these options offer short-term relief by altering antibody levels in the bloodstream.
- Plasmapheresis
This process filters harmful antibodies out of the blood. It’s performed through a central line and typically involves multiple sessions.
- IVIG
This therapy involves infusing high doses of immunoglobulins from healthy donors, which helps to block harmful autoantibodies.
Both are treatments for myasthenia gravis used in:
- Preoperative preparation
- Hospitalised patients in respiratory distress
- Those needing rapid improvement
What Is the Most Effective Treatment for Myasthenia Gravis?
There is no universal answer because the most effective treatment for myasthenia gravis depends on the individual. For some, acetylcholinesterase inhibitors alone are sufficient. For others, a combination of immunosuppressants, surgery, or advanced biologics may be required.
Effectiveness is usually judged by:
- Improved muscle strength
- Reduced flare-ups
- Lower medication requirements
- Better daily functioning
Patients with mild ocular symptoms may manage with pyridostigmine alone. Those with generalised disease often require immunosuppressants or thymectomy. Refractory cases may benefit from monoclonal antibody therapies.
Myasthenia Gravis and Treatment Response: What to Expect
Treatment doesn’t follow a one-size-fits-all path. Regular monitoring, adjustments, and coordination between the patient and a neurologist are essential. Improvements may take weeks or even months, especially with immune therapies.
Managing expectations is important. Most people with treatment myasthenia gravis regain a near-normal quality of life, though flares may still occur.
Lifestyle Support and Additional Therapies
Although medicines are essential, a comprehensive plan includes supportive strategies:
1. Physiotherapy
Helps to maintain mobility and prevent muscle wastage.
2. Speech and Swallow Therapy
Supports safe eating and speaking for those with bulbar involvement.
3. Nutritional Advice
Soft foods and smaller, more frequent meals help reduce fatigue during eating.
4. Emotional and Mental Health Support
Living with a chronic condition can be isolating. Support groups and counselling offer reassurance and community.
For ongoing management, it helps to remain informed and actively engaged with your care. You can read more in our in-depth article on myasthenia gravis and treatment.
FAQs
What is the treatment for myasthenia gravis in older adults?
Older patients may need lower doses of immunosuppressants to avoid complications. IVIG is often preferred during crises due to fewer side effects.
Can myasthenia gravis go into remission?
Yes, particularly after thymectomy. Many achieve partial or full remission with appropriate treatment.
What is the role of biologics in treatments of myasthenia gravis?
Biologics like eculizumab are usually reserved for patients who don’t respond to traditional therapies. They provide targeted immune suppression with fewer generalised effects.
Is exercise safe with myasthenia gravis?
Moderate activity is encouraged but should not lead to fatigue. It’s best to work with a physiotherapist familiar with treatment myasthenia gravis care plans.
Final Thoughts
Choosing the best Herbal Treatment for Myasthenia Gravis means considering the individual’s symptoms, response to medication, and quality of life. The range of options—from symptom relief through to advanced immunotherapy—allows for a personalised, flexible approach.
If you’re looking to explore which myasthenia gravis treatment is most appropriate, consult a neurologist experienced in neuromuscular conditions. A tailored plan can make a significant difference in symptom control and day-to-day wellbeing.
To learn more about new developments in treatments for myasthenia gravis, stay updated with our future posts.
Related Articles:
Myasthenia Gravis Symptoms: What to Watch for and How to Respond
Best Food for Myasthenia Gravis: Eat Well to Support Your Strength
The Evolving Landscape of Autoimmune Disease Research
Home Remedies for Myasthenia Gravis Find the Comfort You Need
Natural and Herbal Treatment for Myasthenia Gravis
Myasthenia Gravis Signs and Symptoms: What You Need to Recognise Early