Magnesium and Myasthenia Gravis: Could This Mineral Hold the Key to Relief?

Myasthenia Gravis (MG) is a rare, chronic autoimmune neuromuscular disorder that causes weakness in the skeletal muscles—the muscles responsible for activities like breathing, speaking, swallowing, and moving the arms and legs. For individuals living with MG, daily life can feel like navigating a series of unpredictable hurdles, as muscle weakness can fluctuate from mild to severely debilitating.
Over the years, researchers and clinicians have explored various treatments aimed at improving quality of life for people with MG. Among the many factors that influence muscle health and nerve transmission, magnesium has emerged as a point of discussion. This raises an important question: What is the connection between magnesium and Myasthenia Gravis, and could this mineral play a role in symptom management or relief?
The delve into the relationship between magnesium and Myasthenia Gravis, review current research, discuss potential benefits and risks, and explore the practical considerations for patients and healthcare providers.
Related Article: Myasthenia Gravis in Children: 10 Signs Parents Should Never Ignore
Understanding Myasthenia Gravis
Myasthenia Gravis (MG) is a chronic autoimmune neuromuscular disorder that causes weakness in the voluntary muscles the muscles you control consciously, such as those used for eye movement, facial expression, chewing, swallowing, and breathing.

1. How It Happens (Underlying Mechanism)
- In MG, the immune system mistakenly produces antibodies that interfere with the communication between nerves and muscles.
- Normally:
- Nerve endings release acetylcholine (a neurotransmitter) at the neuromuscular junction.
- Acetylcholine binds to acetylcholine receptors on the muscle, triggering contraction.
- In MG:
- Antibodies block, alter, or destroy these receptors.
- This reduces the muscle’s ability to contract effectively.
- Over time, the number of working receptors decreases, leading to noticeable muscle weakness.
2. Key Symptoms
The hallmark feature of MG is muscle weakness that worsens with activity and improves with rest (called fatigability).
Commonly affected areas include:
- Eyes and Eyelids
- Drooping eyelids (ptosis)
- Double vision (diplopia)
- Face and Throat
- Difficulty speaking (dysarthria)
- Slurred speech
- Trouble swallowing (dysphagia)
- Difficulty chewing
- Neck and Limbs
- Weak neck muscles (head may droop)
- Weakness in arms and legs
- Breathing
- In severe cases, weakness of breathing muscles can lead to myasthenic crisis a life-threatening emergency requiring immediate medical care.
3. Types of Myasthenia Gravis
- Ocular MG — symptoms limited to the eyes.
- Generalized MG — weakness affects multiple muscle groups.
- Neonatal MG — temporary condition in newborns of mothers with MG (due to transferred antibodies).
- Congenital Myasthenic Syndromes — rare, inherited disorders affecting the neuromuscular junction (not autoimmune).
Related Article: What is the Most Effective Treatment for Myasthenia Gravis?
4. Causes
- Autoimmune origin — the exact trigger is unknown, but immune system dysfunction is central.
- Thymus gland role:
- Many patients have an abnormally large thymus or thymoma (tumor of the thymus).
- The thymus is involved in immune cell development and may contribute to the production of harmful antibodies.
- Demographics:
- Can occur at any age.
- More common in women under 40 and men over 60.
- Not directly inherited, but genetic factors may increase susceptibility.
5. Treatment Options
While there is no cure, Treatment for Myasthenia Gravis can be managed effectively:
- Medications
- Anticholinesterase drugs (e.g., pyridostigmine) — improve communication between nerves and muscles.
- Immunosuppressants — reduce antibody production (e.g., corticosteroids, azathioprine).
- Plasmapheresis and Intravenous Immunoglobulin (IVIG)
- Used in severe cases or crisis to remove/block antibodies quickly.
- Surgery
- Thymectomy — removal of the thymus can improve symptoms, especially in patients with thymoma.
- Supportive measures
- Lifestyle adjustments to avoid fatigue and infections (both can worsen symptoms).
Magnesium: An Essential Mineral
Magnesium is a vital mineral and electrolyte that plays a critical role in hundreds of biochemical reactions in the human body. It is involved in everything from muscle contraction to nerve transmission, and from energy production to maintaining a steady heartbeat. Despite its importance, magnesium deficiency is surprisingly common, often due to poor dietary intake, excessive stress, or certain medical conditions.

Biological Functions
Magnesium is a cofactor in more than 300 enzymatic systems that regulate diverse biochemical processes, including:
- Energy Production: Essential in the synthesis of ATP (adenosine triphosphate), the body’s main energy currency.
- Protein Synthesis: Assists in building and repairing body tissues.
- Nerve and Muscle Function: Regulates muscle contraction, nerve impulse conduction, and helps maintain normal heart rhythm.
- Bone Health: Around 60% of the body’s magnesium is stored in the bones, contributing to their structure and strength.
- Blood Sugar Control: Supports insulin regulation and glucose metabolism.
- Electrolyte Balance: Helps maintain proper levels of potassium, calcium, and sodium.
Recommended Intake
The recommended dietary allowance (RDA) varies by age, sex, and life stage:
- Adult men: ~400–420 mg/day
- Adult women: ~310–320 mg/day
- Pregnant women: ~350–360 mg/day
- Children: Lower amounts depending on age.
Supplementation and Safety
Magnesium supplements are available in several forms, such as magnesium citrate, magnesium glycinate, and magnesium oxide. While generally safe in recommended doses, excessive magnesium intake from Supplements can cause diarrhea, nausea, and abdominal cramping. Very high doses may lead to magnesium toxicity, especially in people with kidney disease.
Health Benefits
Adequate magnesium levels are associated with:
- Reduced risk of type 2 diabetes
- Better blood pressure control
- Lower inflammation markers
- Improved sleep quality
- Reduced migraine frequency
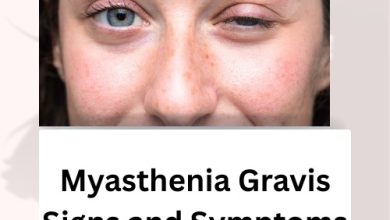
Related Article: Myasthenia Gravis Signs and Symptoms: What You Need to Recognise Early
The Complex Relationship Between Magnesium and Myasthenia Gravis
When people hear the phrase “magnesium and Myasthenia Gravis”, they might assume one of two things:
- That magnesium must be good for the condition, since it’s an essential mineral.
- Or that it’s dangerous, because they’ve heard it can make symptoms worse.
In reality, the connection is more complicated than either assumption suggests.
Magnesium’s Role in Neuromuscular Transmission
Magnesium works in the body as a natural calcium blocker (or “calcium antagonist”). At the neuromuscular junction the place where nerves communicate with muscles—calcium is essential for nerve endings to release a chemical messenger called acetylcholine (ACh). Acetylcholine travels across the junction and binds to receptors on the muscle, telling it to contract.
Magnesium can limit the amount of calcium that enters nerve endings. Less calcium means less acetylcholine is released.
- In healthy people: This is usually helpful. It prevents nerve overexcitation, allows muscles to relax properly after contracting, and protects against muscle cramps or spasms.
- In people with Myasthenia Gravis (MG): The situation is very different. MG is an autoimmune condition in which the acetylcholine receptors on the muscle are damaged or blocked by antibodies. This already reduces the efficiency of nerve-to-muscle communication. If magnesium further reduces acetylcholine release, it can make this communication even weaker—leading to more muscle fatigue, weakness, or even dangerous worsening of symptoms.
Magnesium isn’t inherently “good” or “bad” for everyone with MG it depends on the dose, the person’s health status, and the situation. In some cases, excess magnesium (from supplements, certain medications, or intravenous fluids) can trigger or worsen muscle weakness in MG patients. This is why healthcare providers often approach magnesium use in MG with caution.
Related Article: Myasthenia Gravis Symptoms: What to Watch for and How to Respond
Could Magnesium Ever Be Helpful in Myasthenia Gravis?
While high-dose magnesium can be harmful for some MG patients, that doesn’t mean magnesium is always the enemy. In fact, magnesium deficiency has its own risks, which can include:
- Muscle cramps
- Arrhythmias
- Fatigue
- Neurological symptoms
In certain contexts particularly in MG patients who are magnesium-deficient—carefully monitored supplementation may be beneficial. Here’s why:
- Muscle Function Support: Magnesium is essential for energy metabolism in muscle fibers, helping muscles contract efficiently.
- Nerve Health: Adequate magnesium supports nerve conduction and prevents hyperexcitability.
- Overall Health Maintenance: Deficiency can contribute to other health problems that indirectly worsen MG symptoms, such as poor sleep and cardiovascular strain.
Clinical Observations and Warnings
Medical literature contains reports of magnesium worsening muscle weakness in MG patients, particularly when administered intravenously in high doses, such as in hospital settings for conditions like pre-eclampsia, arrhythmia, or severe asthma.
Examples:
- Intravenous magnesium sulfate has been shown to trigger respiratory muscle weakness in MG patients, occasionally leading to a myasthenic crisis (a medical emergency characterized by severe respiratory weakness).
- Even moderate oral supplementation has raised concerns for individuals who are already borderline in muscle strength.
Because of these findings, many neurology guidelines advise caution with magnesium supplementation in Myasthenia Gravis, especially without medical supervision.
Practical Considerations for Patients and Clinicians
When thinking about magnesium and Myasthenia Gravis, the key is balance neither excessive intake nor severe deficiency is desirable.
1. Assessing Magnesium Status
- Blood tests (serum magnesium levels) can help identify deficiencies, although they don’t always reflect tissue magnesium stores accurately.
- Dietary assessment can reveal whether intake is below the recommended level.
2. Dietary Magnesium vs. Supplements
- Dietary magnesium from whole foods is generally safe, as the body regulates absorption and excretion effectively.
- Supplemental magnesium especially high-dose forms can be risky for MG patients if not medically indicated.
3. Medical Supervision
- Any supplementation should be discussed with a neurologist familiar with MG.
- Hospitalized MG patients should have magnesium administration carefully considered, particularly in IV form.
Related Article: Best Food for Myasthenia Gravis: Eat Well to Support Your Strength
Research Landscape: What Studies Say
Unfortunately, there is limited direct research specifically investigating magnesium supplementation in MG patients. Most evidence comes from:
- Case reports of adverse reactions to intravenous magnesium
- Experimental data on magnesium’s effect on acetylcholine release
- Observational studies linking magnesium status to general muscle and nerve function
A 2018 review in Frontiers in Neurology highlighted that while magnesium toxicity is a concern for MG patients, the relationship is not fully understood. The review emphasized that individualized assessment is essential before deciding on supplementation.
Magnesium-Rich Foods for MG Patients
For most people with Myasthenia Gravis, getting magnesium from natural food sources is the safest way to support general health. Examples include:
| Food Source | Magnesium Content (mg per serving) |
| Pumpkin seeds (1 oz) | 168 mg |
| Almonds (1 oz) | 80 mg |
| Spinach (1 cup cooked) | 157 mg |
| Black beans (1 cup) | 120 mg |
| Mackerel (3 oz) | 82 mg |
| Quinoa (1 cup cooked) | 118 mg |
Note: These amounts contribute to the RDA without approaching levels that might cause neuromuscular suppression.
Magnesium Deficiency in the General Population
Magnesium deficiency is not uncommon, particularly in individuals with:
- Poor dietary habits
- Gastrointestinal disorders (e.g., Crohn’s disease, celiac disease)
- Chronic alcohol use
- Use of certain medications (e.g., proton pump inhibitors, diuretics)
If an MG patient falls into one of these categories, a magnesium deficiency could worsen muscle function indirectly.
Lifestyle Factors That Influence Magnesium Levels
Several lifestyle factors can influence magnesium balance and, indirectly, the conversation about magnesium and Myasthenia Gravis:
- Stress – Chronic stress increases magnesium excretion.
- High sugar intake – Excess sugar can increase magnesium loss in urine.
- Alcohol – Alcohol interferes with magnesium absorption.
- Exercise – Moderate exercise benefits magnesium metabolism, but intense exercise can deplete levels.
For MG patients, balancing these factors is part of overall symptom management.
The Future of Research on Magnesium and Myasthenia Gravis
Given the potential for both benefit and harm, more research is urgently needed to answer key questions:
- What magnesium levels are optimal for MG patients?
- Are certain forms of magnesium safer than others in MG?
- Could targeted magnesium therapy help MG patients with confirmed deficiency without worsening weakness?
Until such data is available, the best approach is personalized care based on individual risk factors, symptoms, and lab results.
Conclusion
The relationship between magnesium and Myasthenia Gravis is a delicate one. On the one hand, magnesium is an essential mineral with undeniable benefits for muscle and nerve health. On the other, excessive magnesium particularly in supplemental or intravenous form can suppress acetylcholine release and worsen the hallmark weakness of MG.
For MG patients, the path forward lies in careful assessment, moderation, and close collaboration with healthcare providers. Magnesium is neither a cure-all nor a universal danger it is a powerful nutrient that, when managed wisely, could be part of a balanced approach to living well with Myasthenia Gravis.
Related Article: The Evolving Landscape of Autoimmune Disease Research