Myasthenia Gravis in Children: 10 Signs Parents Should Never Ignore

Myasthenia Gravis in children is a rare but serious autoimmune neuromuscular disorder that affects the way nerves communicate with muscles. This condition leads to muscle weakness that can worsen with activity and improve with rest. While Myasthenia Gravis (MG) is often associated with adults, it can also appear in infants, toddlers, and adolescents sometimes with subtle symptoms that parents might mistake for fatigue, clumsiness, or even behavioral issues.
Early recognition is vital because prompt diagnosis and treatment can greatly improve a child’s quality of life and prevent life-threatening complications. In this guide, we will explore 10 important signs of Myasthenia Gravis in children that parents should never ignore, along with a deeper understanding of the condition and its implications.
Related Article: What is the Most Effective Treatment for Myasthenia Gravis?
Understanding Myasthenia Gravis in Children

1. What is Myasthenia Gravis?
Myasthenia Gravis (MG) is a chronic autoimmune neuromuscular disorder that causes weakness in the skeletal muscles the muscles your body uses for movement, breathing, and maintaining posture.
- In MG, the body’s immune system mistakenly produces antibodies that interfere with the communication between nerves and muscles.
- Specifically, these antibodies target receptors for a chemical messenger called acetylcholine at the neuromuscular junction, making it difficult for the muscles to contract.
- The key feature of MG is muscle weakness that worsens with activity (fatigability) and improves with rest.
2. Types of Myasthenia Gravis
There are different types, but in children, the most relevant are:
- Congenital Myasthenic Syndromes (CMS) – Genetic (not autoimmune) disorders affecting neuromuscular transmission from birth.
- Juvenile Myasthenia Gravis (JMG) – Autoimmune MG that develops in childhood or adolescence.
- Transient Neonatal Myasthenia Gravis – Temporary MG in newborns caused by antibodies crossing the placenta from a mother with MG; symptoms usually resolve within weeks.
3. Why is it Different in Children?
While MG is more common in adults, in children it:
- May present earlier and sometimes mimic other conditions like muscular dystrophy.
- Often requires careful diagnosis because children can’t always explain fatigue well.
- May have a stronger link to genetic factors (especially in congenital forms).
4. Causes in Children
- Autoimmune (Juvenile MG): The child’s immune system produces antibodies that block or damage acetylcholine receptors.
- Genetic (CMS): Inherited mutations affect proteins essential for nerve-muscle communication.
- Maternal Antibody Transfer: Antibodies pass from mother to newborn during pregnancy.
5. Common Symptoms in Children
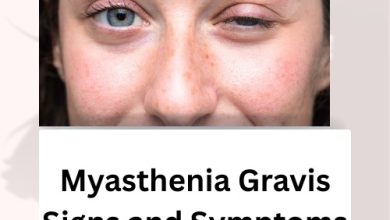
- Drooping eyelids (ptosis)
- Double vision (diplopia)
- Weak facial muscles — may cause a flat expression or difficulty smiling
- Trouble speaking clearly (dysarthria)
- Difficulty chewing or swallowing (dysphagia)
- Weakness in neck, arms, or legs
- Worsening symptoms with activity and improvement with rest
Related Article: Myasthenia Gravis Signs and Symptoms: What You Need to Recognise Early
The 10 Signs Parents Should Never Ignore
Myasthenia Gravis (MG) is a rare autoimmune condition that affects the communication between nerves and muscles, causing weakness that worsens with activity and improves with rest. In children, symptoms can be subtle at first and may come and go, making them easy to overlook. Early recognition is key to proper diagnosis and treatment.
Below are 10 signs parents should watch for, explained in detail with practical examples.
1. Persistent Eyelid Drooping (Ptosis)
One of the earliest and most noticeable signs of MG is ptosis drooping of one or both eyelids.
What to look for:
- The droop becomes more obvious in the late afternoon or after school.
- Your child tilts their head back or raises their eyebrows to see better.
- In photos, one eyelid may look lower than the other.
Because ptosis may improve after rest, parents sometimes assume it’s just tiredness. But if the droop appears every day or worsens with activity, it should be evaluated by a doctor.
2. Double Vision (Diplopia)
MG can weaken the muscles that keep the eyes aligned, leading to double vision but children may not know how to describe it.
Possible signs:
- Squinting, closing one eye, or covering one eye to focus.
- Complaints of blurry or “shadowed” vision.
- Trouble reading, catching a ball, or focusing on distant objects.
Double vision often gets worse after tasks that require prolonged visual focus, such as homework or screen time.
3. Facial Weakness
Facial muscles can be affected, changing a child’s natural expressions.
What parents might see:
- A flat, “mask-like” face with less emotion showing.
- An uneven or weak smile.
- Difficulty making certain expressions—smiling, frowning, or closing the eyes tightly.
- Trouble with actions like puffing cheeks, blowing up balloons, or whistling.
These changes may be gradual, so comparing older and newer photos can be revealing.
4. Difficulty Swallowing (Dysphagia)
Weak throat muscles make swallowing hard and may cause:
- Coughing or choking while eating or drinking.
- Taking unusually long to chew food.
- Choosing soft foods or liquids over solids.
- Gagging or spitting out certain foods.
Severe swallowing problems can cause aspiration (food or drink entering the airway), which can lead to pneumonia and requires urgent medical attention.
5. Slurred or Nasal Speech
Speech changes can be subtle but important.
Possible clues:
- Words become slurred, especially after talking for a while.
- Voice sounds nasal, as if the child has a cold, but without other cold symptoms.
- Teachers or friends notice the child is harder to understand.
This may be mistaken for shyness or mumbling, but when it fluctuates during the day, it can signal MG.
6. Weak Neck Muscles (Head Drop)
Neck muscle weakness can make it hard for the child to hold their head up.
- Head may tilt forward, especially toward the end of the day.
- Child might support their head with a hand while reading or using a tablet.
- Neck may look awkward in photos or when sitting in class.
This can also contribute to poor posture and neck discomfort.
7. Limb Weakness
MG-related limb weakness often shows up during active play or sports.
Signs include:
- Trouble climbing stairs, running, or jumping.
- Needing help to get up from the floor or from sitting.
- Avoiding physical activities they used to enjoy.
- Fatigue after a short walk or brief playtime.
If a usually active child suddenly prefers sitting activities, it’s worth noting.
8. Rapid Muscle Fatigue
This is a hallmark of MG—weakness that comes on quickly with use but improves with rest.
- Weakness appears after even mild activity, such as writing, chewing, or walking.
- Rest restores strength, but the weakness comes back once the activity resumes.
This “on–off” pattern is very different from the steady tiredness of normal fatigue.
9. Breathing Difficulties
In rare but severe cases, MG affects the muscles used for breathing.
Warning signs:
- Shortness of breath or shallow breathing, especially when lying down.
- Struggling to finish a sentence without pausing for breath.
- Frequent sighing or gasping.
This can become a myasthenic crisis, which is a life-threatening emergency. If breathing becomes difficult, seek immediate medical help.
10. Fluctuating Symptoms
The most distinctive feature of MG is that symptoms vary in severity.
- Child may seem stronger in the morning and noticeably weaker by evening.
- Weakness worsens after exercise and improves with rest.
- Symptoms can disappear for days, then return suddenly.
Keeping a symptom diary—time of day, activities before symptoms can help doctors recognize this pattern.
If you notice a combination of these symptoms—especially ones that get worse with activity and improve with rest—it’s important to consult a doctor, ideally a neurologist familiar with pediatric MG. Early diagnosis can make a significant difference in treatment and quality of life.
Related Article: Myasthenia Gravis Symptoms: What to Watch for and How to Respond
Why These Signs Are Often Missed
Myasthenia Gravis in children can be overlooked because:
- Symptoms mimic common childhood issues like laziness, clumsiness, or poor attention span.
- Fluctuating weakness can confuse both parents and healthcare providers.
- Rare disease status means many general practitioners see very few cases in their career.
Awareness among parents is crucial for prompting timely specialist referrals.
Possible Causes and Risk Factors in Children
While the exact cause of autoimmune Myasthenia Gravis is not fully understood, contributing factors may include:
- Genetic predisposition – Family history of autoimmune diseases.
- Immune system dysregulation – Triggering the production of harmful antibodies.
- Associated conditions – Some children may have an enlarged thymus gland.
Treatment Options for Myasthenia Gravis in Children
Treatment for Myasthenia Gravis in Children plans are highly individualized but may include:
1. Medications
- Anticholinesterase drugs (e.g., pyridostigmine) to improve nerve-muscle communication.
- Immunosuppressants to reduce antibody production.
- Steroids for controlling immune activity during flare-ups.
2. Thymectomy
In some cases, surgical removal of the thymus gland can improve symptoms.
3. Plasmapheresis or Intravenous Immunoglobulin (IVIG)
These are rapid-acting therapies used during severe flare-ups or crises.
Related Article: Best Food for Myasthenia Gravis: Eat Well to Support Your Strength
Living with Myasthenia Gravis in Children
Daily management often includes:
- Energy conservation – Planning activities with rest breaks.
- Balanced nutrition – Preventing swallowing difficulties from causing malnutrition.
- School accommodations – Extra time for tests, lighter homework load, or physical activity adjustments.
- Emotional support – Counseling for children coping with chronic illness.
Parents play a key role in advocating for their child’s needs both at home and in school.
Parental Tips for Early Detection
- Keep a symptom diary noting time of day and activity level.
- Record short videos of fluctuating weakness to show doctors.
- Compare old photos to see if eyelid drooping or facial changes have appeared gradually.
- Trust your instincts if something seems off, push for specialist evaluation.
Related Article: The Evolving Landscape of Autoimmune Disease Research
Conclusion
Myasthenia Gravis in children is a challenging condition, but with awareness, early diagnosis, and proper treatment, many children can lead active, fulfilling lives. The 10 signs outlined above especially when they appear in combination and fluctuate during the day should prompt parents to seek medical advice promptly.
The key takeaway is simple: never dismiss unusual or persistent weakness as “just tiredness” in a child. By recognizing the subtle but telling signs of Myasthenia Gravis, parents can be the first and most important advocates in their child’s journey to diagnosis and care.
Related Article: Magnesium and Myasthenia Gravis: Could This Mineral Hold the Key to Relief?