The Evolving Landscape of Autoimmune Disease Research

Autoimmune diseases have long puzzled scientists and clinicians. Over the past decade, however, research into these conditions has advanced at a steady pace, offering greater insight into how and why the body’s immune system begins to attack its own tissues. For patients and caregivers alike, these developments have led to more accurate diagnoses, a wider range of treatment options, and a deeper understanding of disease mechanisms.
What Are Autoimmune Diseases?
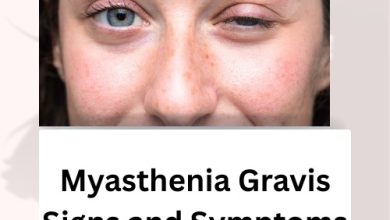
Autoimmune diseases occur when your immune system mistakenly identifies healthy cells as threats. This can lead to inflammation, organ damage, and a wide variety of symptoms that differ depending on the condition. Some of the most recognised autoimmune disorders include rheumatoid arthritis, systemic lupus erythematosus, multiple sclerosis, and Myasthenia Gravis.
Shifting Perspectives on Causes and Triggers
Historically, autoimmune diseases were considered largely genetic. Today, researchers recognise that multiple factors contribute — including environmental exposures, infections, and hormonal influences. For instance, the role of the gut microbiome has gained attention. An imbalance in gut bacteria may contribute to immune dysregulation, making it a promising area for future intervention.
Advances in genome-wide association studies (GWAS) have also pinpointed genetic variants linked to higher risk. This means doctors may eventually be able to assess someone’s likelihood of developing certain autoimmune diseases before symptoms even appear.
Related Article: Natural and Herbal Treatment for Myasthenia Gravis
Breakthroughs in Diagnosis
One of the most meaningful shifts in autoimmune disease research has been the improvement of diagnostic methods. Conditions that once took years to confirm can now be identified more accurately and earlier in their course. This is particularly true for conditions like Myasthenia Gravis, where researchers have improved the detection of specific autoantibodies involved in the disease. If you’re looking to better understand how clinicians confirm this condition, you can learn more in our detailed article on how to Diagnose Myasthenia Gravis.
Emerging diagnostic tools now include advanced imaging techniques, cell-based assays, and AI-supported symptom pattern recognition. These innovations are helping clinicians differentiate between similar conditions and personalise treatment plans sooner.
Treatment Is Becoming More Targeted
Treatment strategies for autoimmune diseases have moved beyond general immune suppression. While corticosteroids and immunosuppressants are still used, newer therapies aim to target specific components of the immune response.
Biologic drugs, such as monoclonal antibodies, have become standard in many autoimmune conditions. These therapies are designed to block the activity of molecules like TNF-alpha or interleukins that play a key role in inflammation. More recently, Janus kinase (JAK) inhibitors have shown promise in conditions such as rheumatoid arthritis and alopecia areata.
Patients with Myasthenia Gravis, for example, may benefit from complement inhibitors — a newer class of medication that can reduce symptoms by limiting a part of the immune system’s attack mechanism.
Personalised Medicine Is on the Horizon
No two patients experience autoimmune disease the same way. Researchers are now working towards more personalised approaches to care, combining genetics, lifestyle factors, and individual immune profiles to tailor treatments.
Biomarker research is central to this effort. Identifying reliable markers in the blood or tissue may help predict flares, treatment response, or disease progression. This will be especially useful in diseases where symptoms fluctuate or where treatment needs to be adjusted frequently.
The Role of Clinical Trials
Ongoing clinical trials are essential to this progress. These studies test new therapies and combinations, explore different dosing schedules, and evaluate safety and long-term outcomes. Patients who participate in trials not only gain access to cutting-edge treatments, but also contribute to expanding knowledge for future generations.
Some trials are even exploring whether certain autoimmune diseases can go into long-term remission with early, aggressive treatment — potentially reducing the need for life-long medication.
What This Means for Patients and Families
For those living with autoimmune diseases, this evolving research landscape offers real hope. Earlier diagnoses mean fewer years of unexplained symptoms. Better-targeted treatments mean fewer side effects and better quality of life. And the push towards personalised medicine holds the promise of care that adapts to your unique needs, not just the name of your diagnosis.
Patients and caregivers are encouraged to stay informed about new research developments, speak regularly with their healthcare providers about treatment options, and consider participating in registries or research studies when possible.
Conclusion
Autoimmune disease research continues to move forward, bringing renewed focus on earlier diagnosis, more effective treatment, and long-term management. Myasthenia Gravis and other conditions serve as examples of how sustained scientific effort is improving lives. As research expands, so do the possibilities for living well with these challenging conditions.
For more on how specific autoimmune diseases are identified, read how clinicians Diagnose Myasthenia Gravis using the latest methods.